Recognizing tetanus risks can save your life after a puncture wound. Tetanus, caused by Clostridium tetani, turns serious without prompt action. Puncture wounds offer the anaerobic conditions this bacteria needs. Symptoms like lockjaw and muscle stiffness signal danger. Prevention through vaccination is vital, but if a wound happens, immediate cleansing and medical consultation are key. Early treatment with tetanus antitoxin can stop the toxin. Also, keeping vaccinations up-to-date, including booster shots every 10 years, offers continued protection. Recognizing symptoms and acting fast vastly improves outcomes. Discovering how to spot and respond to these signs could be the difference between a full recovery and severe complications.
Listen to the Article
Key Takeaways
- Early recognition of tetanus symptoms enables prompt medical intervention.
- Awareness of tetanus risks encourages immediate wound cleansing and care.
- Recognizing risks promotes timely tetanus vaccination or booster administration.
- Knowledge of soil contamination risks informs safer handling of puncture wounds.
- Understanding tetanus signs improves quick decision-making for seeking medical help.
Understanding Tetanus
Tetanus, often stemming from puncture wounds, is a serious bacterial infection that affects your nervous system, potentially leading to life-threatening muscle spasms. When the bacteria, Clostridium tetani, enter your body, they release a toxin called tetanospasmin. This toxin interferes with your nerve impulses, causing muscles to tighten uncontrollably. The jaw muscle is frequently affected first, leading to the characteristic ‘lockjaw‘ symptom. However, the spasms can rapidly spread, affecting the respiratory muscles and posing a fatal risk without prompt treatment.
Understanding the mechanism of this infection is crucial for anyone dedicated to serving others, especially in healthcare or emergency response roles. Recognizing the early signs of tetanus, such as muscle stiffness, difficulty swallowing, and spasms, can significantly improve the outcomes for those affected. Quick identification and administration of treatment, including tetanus antitoxin, can halt the progression of the disease.
It’s imperative to remember that tetanus can be prevented through vaccination. As someone committed to the well-being of others, advocating for and ensuring up-to-date vaccinations in your community serves as a powerful tool in preventing this potentially deadly infection.
Common Sources of Infection
Understanding the various environments where the Clostridium tetani bacterium thrives is crucial in identifying the common sources of tetanus infections. This bacterium is commonly found in soil, dust, and manure, making outdoor environments particularly risky. However, it’s not just the natural earth that poses a risk; objects that come into contact with these elements can also harbor the bacterium. Rusty nails, gardening tools, and even animal bites can be potential sources of infection.
In your efforts to serve others, especially in outdoor or agricultural settings, it’s important to recognize these risks. Puncture wounds are particularly susceptible to tetanus infections because the bacterium thrives in anaerobic (oxygen-free) conditions, such as the deep, narrow channels created by such injuries.
Preventative measures, like wearing protective footwear and gloves, can significantly reduce the risk of exposure. However, awareness is key. If someone sustains a puncture wound, understanding that even a minor injury can be a conduit for infection emphasizes the need for prompt and appropriate response. This knowledge not only protects those you’re serving but empowers them to take preventive steps in their daily lives, reducing the overall burden of tetanus infections.
Importance of Immunization Status
You must recognize that the effectiveness of the tetanus vaccine diminishes over time, necessitating periodic updates to your immunization records. Keeping these records current is crucial not only for your health but also plays a significant role in sustaining herd immunity, which protects those who can’t be vaccinated.
Understanding the impact of herd immunity underscores the collective responsibility we share in preventing outbreaks of vaccine-preventable diseases like tetanus.
Vaccine Effectiveness Over Time
Considering the fluctuating levels of protection it offers, staying updated on your tetanus vaccination status is critical for effective defense against infection.
The efficacy of the tetanus vaccine diminishes over time, necessitating booster shots to maintain immunity. Initially, a series of vaccinations starts in childhood, but protection doesn’t last indefinitely. Adults require a booster every 10 years to ensure continuous protection.
It’s not just about personal health; it’s about community safety. When you’re protected, you’re less likely to contribute to the spread of this potentially deadly bacteria.
Understanding the mechanism and timeline of vaccine effectiveness empowers you to take proactive steps in your healthcare, ultimately serving not just yourself but those around you by upholding herd immunity and preventing outbreaks.
Updating Immunization Records Regularly
Given the necessity of booster shots every 10 years to maintain immunity against tetanus, keeping your immunization records up-to-date plays a pivotal role in your healthcare management. This diligence ensures you’re protected when exposed to potential tetanus infections, especially through puncture wounds.
An accurate record provides healthcare professionals with essential information, allowing for swift, appropriate interventions, thereby minimizing risks and complications. Moreover, it empowers you to make informed decisions about your health and the well-being of those you serve.
Regularly reviewing and updating your immunization status isn’t just a personal health measure; it’s a responsibility towards community welfare. By maintaining vigilance over your immunization history, you contribute to a safer, healthier environment for everyone.
Understanding Herd Immunity Impact
A community’s overall health significantly benefits from high immunization rates, as they foster herd immunity, reducing the spread of infections like tetanus. Herd immunity occurs when a large portion of a community becomes immune to a disease, making its spread from person to person unlikely.
This protection is crucial, especially for those who can’t receive vaccines due to medical conditions. By maintaining your immunization status, you’re not just protecting yourself; you’re safeguarding the entire community from potential outbreaks.
It’s a collective shield against diseases, underlining the importance of every individual’s role in public health. Therefore, keeping your tetanus vaccinations up to date isn’t an individual choice—it’s a societal responsibility.
Each shot strengthens the community’s defense, saving lives by preventing the spread of deadly infections.
Recognizing Symptoms Early
Early recognition of tetanus symptoms can significantly improve treatment outcomes, making it crucial for you to understand the initial signs, such as muscle stiffness and spasms, that often begin in the jaw. Beyond these initial manifestations, the progression of symptoms can be rapid and severe, underscoring the importance of swift action.
As tetanus progresses, you might notice an increase in body temperature and sweating. These signs, while seemingly common to many conditions, can indicate the body’s struggle against the tetanus toxin. Sweating and fever, in the context of a recent puncture wound, should prompt an immediate consultation with healthcare professionals.
Additionally, difficulty swallowing and stiffness in the neck muscles can develop. These symptoms reflect the toxin’s spread and its effect on the nervous system, leading to generalized muscle rigidity. Recognizing these signs early on can be lifesaving, particularly in environments where access to medical care might be delayed.
Understanding these symptoms allows you to serve those in your community by ensuring swift and informed responses to potential tetanus infections. Your knowledge can bridge the critical gap between infection and treatment, fundamentally altering the course of recovery for those affected.
Muscle Stiffness and Jaw Locking
Muscle stiffness, particularly in the jaw area leading to lockjaw, stands as a hallmark symptom of tetanus, necessitating prompt medical attention. This condition, scientifically referred to as trismus, often signifies the onset of a serious bacterial infection that thrives in environments devoid of oxygen, such as puncture wounds. When you’re informed about the risks and symptoms of tetanus, you’re better equipped to serve and protect your community, especially those most vulnerable.
Consider the following to truly grasp the gravity of the situation:
- Immediate Pain: The initial discomfort mightn’t seem alarming, but tetanus bacteria can rapidly multiply, leading to severe complications.
- Progressive Symptoms: Muscle stiffness doesn’t just stop at the jaw. It can spread, crippling the body’s ability to move freely, creating a state of constant agony.
- Irreversible Damage: Without timely intervention, the consequences of tetanus can lead to long-term health issues, or worse, be fatal.
Understanding the severity of these symptoms emphasizes the importance of recognizing tetanus early. Your knowledge and swift action can significantly alter the course of this disease, turning a potentially devastating situation into a manageable one.
The Role of Booster Shots
Understanding the severe symptoms of tetanus underscores the importance of booster shots in preventing this potentially fatal disease. Tetanus, a life-threatening condition triggered by the bacterium Clostridium tetani, can lead to severe muscle stiffness and jaw locking, among other symptoms. By maintaining up-to-date tetanus immunizations, you’re not just protecting yourself; you’re safeguarding those around you, especially the vulnerable who might be at higher risk.
Booster shots play a crucial role in sustaining your body’s immunity against tetanus. The initial vaccine series isn’t a lifelong shield; your immunity wanes over time, which is why boosters are necessary. Typically, adults should receive a tetanus booster every 10 years, but in the case of a puncture wound or a deep cut, an immediate booster might be required if your last shot was over five years ago.
This proactive approach isn’t just about individual health; it’s a community safeguard. In environments where helping and caring for others is paramount, staying vigilant about booster shots ensures that you remain capable of serving without inadvertently becoming a vector for disease transmission. It’s a simple, yet profoundly impactful, way to contribute to communal well-being.
Soil Contamination Risks
Soil, often overlooked as a mere foundation beneath our feet, harbors the dangerous bacterium Clostridium tetani, posing significant tetanus infection risks through puncture wounds. Understanding the relationship between soil contamination and tetanus is crucial for preventing potentially fatal infections. The spores of C. tetani thrive in soil, especially in environments rich in organic matter. When you’re assisting others, especially in rural or outdoor settings, recognizing these risks becomes vital.
The pathways through which C. tetani enters the body, primarily through puncture wounds, demand vigilant attention. Here’s why:
- Soil acts as a reservoir for tetanus spores. The ubiquity of soil means that even minor injuries can become gateways for infection.
- Tetanus spores can survive for years. Their resilience in soil complicates prevention efforts, necessitating continuous awareness and education.
- The risk is universal. Tetanus spores don’t discriminate by geography or climate, making global vigilance essential.
For those dedicated to serving others, acknowledging these risks empowers you to take proactive steps in wound management and education, fostering a safer environment for everyone involved. Your role in recognizing and addressing soil contamination risks can save lives, emphasizing the importance of detailed, authoritative knowledge in tetanus prevention.
Proper Wound Care Techniques
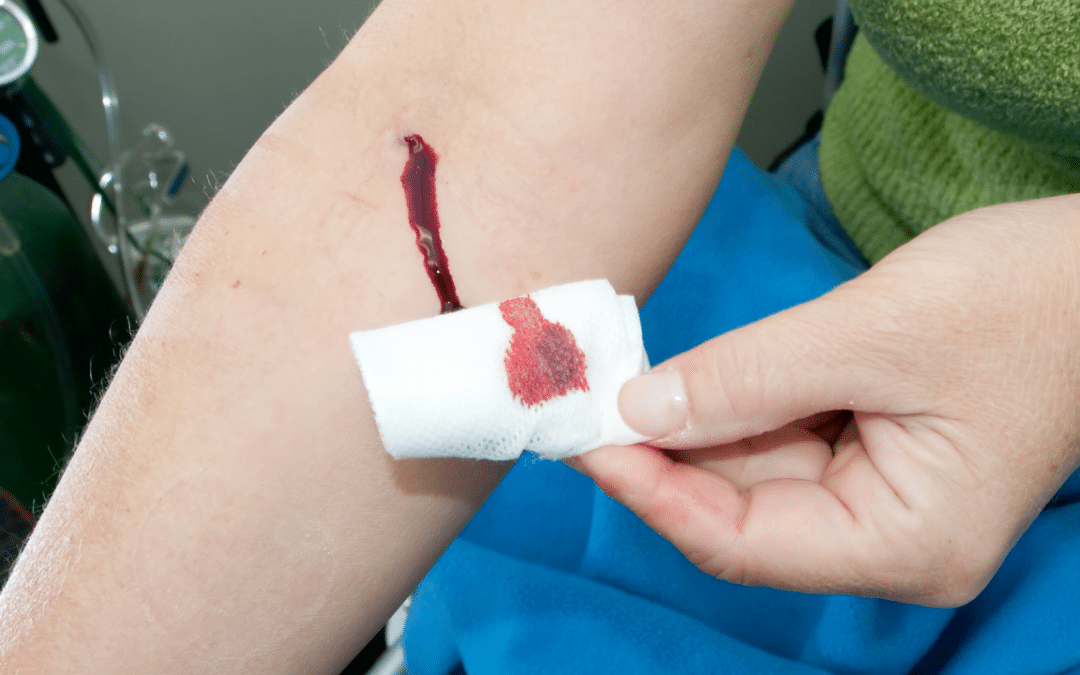
To mitigate the risks of tetanus infection following a puncture wound, it’s crucial you engage in meticulous wound care practices immediately. First, cleanse the wound thoroughly with soap and water. This step is fundamental in removing any contaminants, including bacteria that could cause tetanus. It’s essential to be gentle yet thorough, ensuring all foreign materials are washed away.
Next, apply an antiseptic solution or cream to the wound. This acts as a barrier against infection, further protecting the wound from harmful bacteria. It’s critical to choose a product that’s effective against a broad range of pathogens to ensure maximum protection.
After applying antiseptic, cover the wound with a sterile bandage. This not only keeps the area clean but also prevents additional bacteria from entering the wound. It’s important to change the bandage regularly, especially if it becomes wet or dirty, to maintain a clean environment conducive to healing.
Emergency Response Steps
If you sustain a puncture wound, promptly assessing the situation and recognizing when to seek emergency medical attention becomes critical in preventing tetanus infection. The bacteria that cause tetanus can enter your body through even a minor puncture wound, making vigilance essential. Immediate actions can significantly reduce the risk of developing this potentially fatal disease.
Consider these emergency response steps:
- Evaluate the wound’s depth and severity. Deep or dirty wounds, especially those caused by non-sterile objects, are more susceptible to tetanus bacteria.
- Clean the wound immediately. Washing the wound with soap and water can remove foreign material and bacteria. However, don’t delay professional medical evaluation even if the wound appears clean.
- Seek medical attention without delay. This is crucial, particularly if:
- The wound is deep or contaminated with soil or saliva.
- You can’t recall your last tetanus shot or it has been over 10 years.
- The wound shows signs of infection such as redness, swelling, warmth, or pus.
Analyzing the wound carefully and taking decisive action not only serves your health but also embodies a commitment to safeguarding the well-being of others by preventing the spread of infection.
Vaccination and Prevention Strategies
Understanding the importance of vaccinations and adopting preventative strategies are your best defenses against the risks posed by tetanus in the aftermath of a puncture wound. It’s crucial to recognize that tetanus, a potentially life-threatening condition, can be effectively prevented through vaccination. The tetanus vaccine, typically administered as part of the DTaP or Tdap series, offers robust protection. You’re advised to keep your vaccination status up to date, with booster shots recommended every 10 years for adults.
In addition to vaccination, adopting meticulous wound care practices plays an essential role in prevention. Immediately cleaning and disinfecting any puncture wound, no matter how minor it may seem, drastically reduces the risk of tetanus spore infection. Employing protective gloves and sterile equipment when handling such injuries not only safeguards the injured but also those providing aid.
Furthermore, education on the importance of these preventive measures, especially in communities with limited healthcare access, can significantly diminish tetanus infection rates. By empowering yourself and others with knowledge and resources for proper vaccination and wound care, you’re contributing to a broader culture of health and safety, effectively reducing the global burden of tetanus.
Frequently Asked Questions
How Does Tetanus Affect Pregnant Women and Newborns Differently From the General Population?
You’ll find that tetanus poses a higher risk to pregnant women and newborns, leading to complications like miscarriages and neonatal tetanus, which can be fatal. Understanding these risks helps in providing targeted care and prevention strategies.
Can Natural Remedies or Alternative Medicine Play a Role in Treating Tetanus, or Should They Be Avoided?
You should avoid relying solely on natural remedies for tetanus. While some may offer support, they can’t replace vaccines and medical treatments that are proven lifesavers. It’s critical to prioritize established healthcare practices.
How Does the Body’s Immune Response to a Tetanus Vaccine Change as One Ages?
As you age, your body’s immune response to the tetanus vaccine weakens, making booster shots crucial to maintain protection. It’s essential to stay vigilant with vaccinations to serve and safeguard your community effectively.
Are There Any Documented Cases of Tetanus Infection Despite Complete Vaccination – What Could Cause This Anomaly?
Yes, there have been rare cases of tetanus infection despite full vaccination, like a well-fortified castle breached. This anomaly can stem from immune system weaknesses or improper vaccine storage and handling.
How Does Tetanus Infection Risk Vary by Geographic Location or Climate Conditions?
You’ll find that tetanus risk varies globally, heavily influenced by climate and geography. Warmer, more humid areas increase bacteria survival, raising infection chances. Understanding these variations helps you better serve those in need of guidance.